Conference Posters
These conference posters are preliminary pieces of work that have not been peer-reviewed.
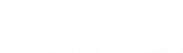
The management of rectal cancer in older patients in England
Presented at the Society of Surgical Oncology Annual Cancer Symposium 2019.
Abstract:
Background - There is significant debate around the treatment of older patients with rectal cancer, with both under and over treatment frequently reported as negatively impacting on the survival of this group. This study sought to examine the use of major surgical resection for rectal cancer in relation to age across the English NHS.
Methods - Data for patients diagnosed with a first primary rectal cancer between 1st April 2009 and 31st December 2014 were obtained from the CORECT-R data repository. Patients were divided into three groups in relation to their age at the time of diagnosis; <70, 70-79 and ≥80. Descriptive analyses were undertaken to assess the variation in treatment and outcomes. Logistic regression models were used to assess the relationship between age, major resection and post-operative outcomes.
Results - In total, 52,922 people were diagnosed with a first primary rectal cancer in England over the study period. The proportion undergoing a major resection decreased with age, falling from 66.5% to 31.7% between patients aged <70 and those aged ≥80. Whilst stoma creation rates were comparable between age groups, reversal within 18 months decreased with age, from 66.3% amongst those aged <70 to 32.4% amongst those aged ≥80.
After adjustment for case-mix factors the odds of 30-day post-operative mortality or a prolonged length of inpatient stay (≥21 days) significantly higher amongst the oldest patient group compared to the youngest. Variation between NHS Trusts in the use of major resection amongst the oldest patients remained after adjustment for casemix factors such as stage of disease. Results from adjusted logistic regression models showed no significant difference in 30-day post-operative mortality, length of stay or emergency readmission amongst those aged 80 and over between Trusts with high and low operative rates. The probability of death due to cancer was comparable across all age groups.
Conclusions - This study demonstrates that older patients who receive a major resection for their rectal cancer have outcomes comparable to the youngest group. However older patients are significantly less likely to undergo this surgery. This significant variation could not be entirely explained by differences in measured characteristics.
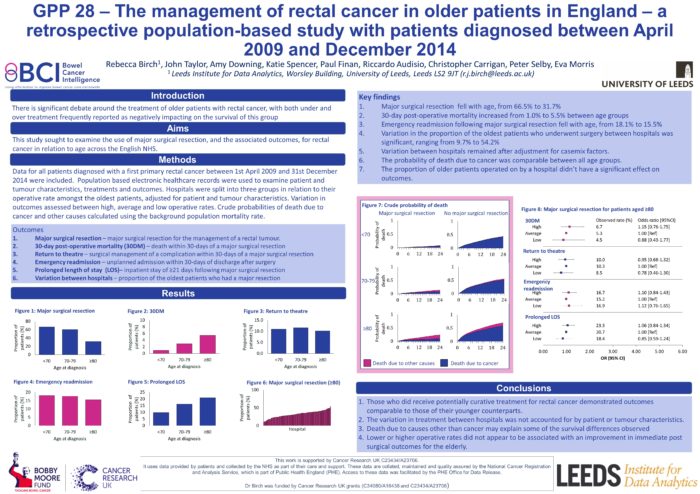
Thirty-day mortality after major surgical resection for rectal cancer amongst elderly patients in England (2009-2014)
Presented at the Association of Coloproctology of Great Britain and Ireland 2019 Annual Meeting.
Abstract:
Background - Surgical resection remains the mainstay of treatment for rectal cancer but its use amongst elderly patients (≥85 years) remains contentious. This study seeks to examine 30-day postoperative mortality (POM) rates following major rectal cancer surgery and to identify which factors are of particular significance amongst the elderly.
Methods - This retrospective, population-based, study included all patients undergoing a major surgical resection for rectal cancer within the English NHS between 2009 and 2014. Descriptive analyses were undertaken to assess the characteristics associated with post-operative mortality. Logistic regression analyses were used to determine the impact of age after adjustment for other factors.
Results - The cohort comprised of 31,884 patients. Patients were grouped by age (<70, 70-74, 75-79, 80-84, 85+). Overall 2.2% of patients died within 30 days of surgery, with an increase from 1.0% in those aged <70 to 8.5% in those aged ≥85. Amongst the oldest patients (≥85), those who underwent surgery within 48 hours of an emergency admission had a POM of 25.0%, however emergency surgery accounted for only 9.1% of this elderly group. Amongst those who received elective surgery the POM was 6.2%, rising to 9.9% amongst males and 9.6% amongst those with one or more comorbidities.
Conclusion - Elderly patients who underwent emergency surgery were identified as a high-risk group in relation to POM, however this subgroup account for a very small proportion of those aged ≥85. For those operated on electively the POM was lower than that which is often quoted as reason not to operate on elderly patients, with only 6.2% of those aged ≥85 dying within 30 days of an elective procedure.
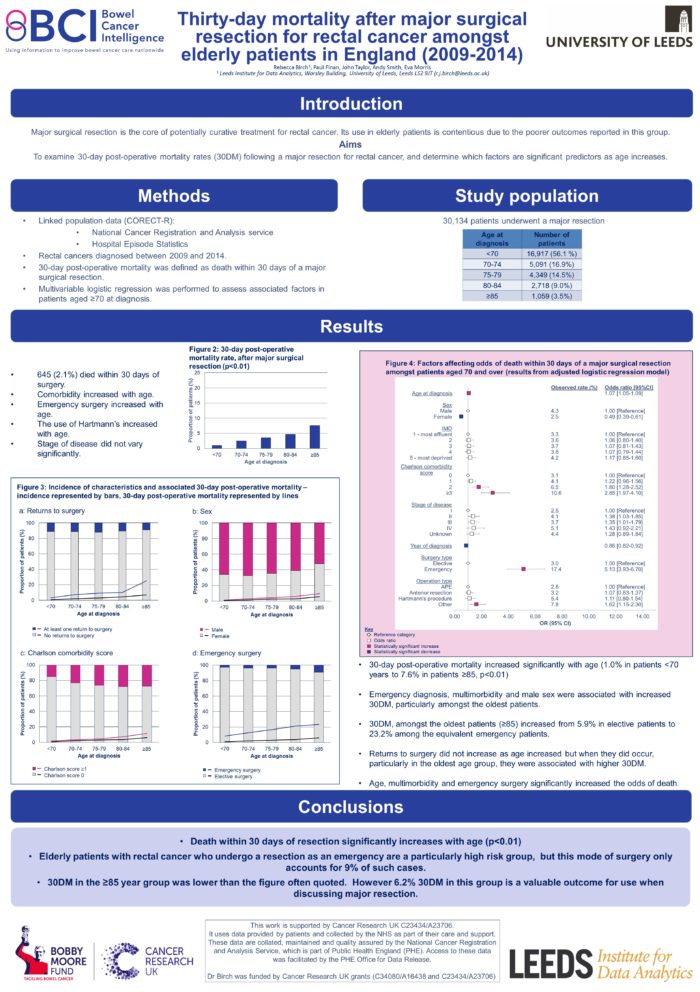
Return to surgery and failure to rescue following major resection for colorectal tumours in the English NHS 2009-2014
Presented at the 38th Congress of the European Society of Surgical Oncology.
Abstract:
Background - Major resectional surgery remains the mainstay of treatment for colorectal cancer (CRC). Returns to theatre after surgery, and failure to rescue (FTR) are used as indicators of quality of care. This population-based study used administrative data to quantify returns to surgery and FTR in CRC patients across England. It assesses differences between key patient groups, variation over time and across NHS trusts.
Materials & Methods - Using linked National Cancer Registration and Hospital Episode Statistics data, CRC patients undergoing a major resection, between 2010-2014, were identified. Details of returns to theatre within thirty days of resection were extracted. FTR was calculated as deaths within 30 days of primary resection in those who were returned to theatre.
Results - Of 118,714 patients undergoing a major resection, 8.2% returned to theatre at least once within 30 days. Returns were more common in patients with rectal tumours (10.9%) than patients with either colonic (7.1%) or rectosigmoid (8.2%) tumours. Returns were less common in the elderly (6.76%), and more frequent in men (9.4%).
Nationally, returns remained stable between 2010-2013 but fell to 7.4% in 2014. In contrast FTR has fallen each year from 9.5% in 2010 to 7.3% in 2014. Between Trusts, returns to theatre ranged from 2.5%-14.6% (IQR 2.2), and FTR from 0-23.3% (IQR 3.2).
Conclusions - Both returns to theatre and FTR can be estimated from national administrative data for CRC patients, and show trends in time and between patients and Trusts. This demonstrates the utility of both as indicators of quality of care in England.
Funnel plots and flexible parametric models: colorectal cancer survival estimation
Presented at LASR 2019 - Big Data: On Time and Space conference.
Abstract:
Colorectal cancer is the 4th most common cancer in the UK with significantly lower survival than in many other comparable countries. As a result, significant efforts are being made to understand the survival disparities and data are required comparing clinical outcomes between the multidisciplinary teams (MDT) that manage the disease within the National Health Service (NHS). Up-to-date relevant statistical methodologies are needed to robustly analyse the complex datasets available, to take into account the differences in characteristics, management and workload across MDT populations, handle missing data related to important factors such as stage of disease and produce robust and meaningful comparisons of care.
Flexible parametric approach was used to estimate survival of patients diagnosed with colorectal cancer. These models allow more complex modelling of relative survival than the more traditional Cox proportional hazards (PH) or other parametric models. They allow more accurate prediction and modelling of excess mortality alongside the ability to adjust for covariates and time-varying effects. The methods were compared using data from National Cancer Registration and Analysis Service (NCRAS). Additionally, other methods used, like multiple imputation (to impute missing stage information) and funnel plots (graphs used to identify outlier performance) will be presented.
Colorectal cancer survival in England
Presented at the Public Health England Cancer Services, Data and Outcomes Conference 2018.
Abstract:
Background- Colorectal cancer (CRC) is the fourth most common cancer in the UK resulting in over 16,000 deaths annually. CRC survival is significantly lower in England than in many other comparable countries, thus efforts are being made to improve results. Equally there is a growing demand for the NHS to publish data on clinical outcomes. This current study aims to investigate national patterns of CRC survival in England.
Method- All individuals, diagnosed with a first primary CRC between 2005 and 2013 and followed-up until the end of 2016, were identified within the linked National Cancer Registration and Hospital Episode Statistics data available from the Bowel Cancer Intelligence Hub. Crude three-year survival rates from diagnosis and from major resection (MR) were estimated both separately (by site of tumour, period of diagnosis, hospital Trust) and overall.
Results- 355,992 individuals were diagnosed with a first primary colorectal cancer over the study period and 211,459 (59%) had a major resection. Overall three-year survival rate increased over time with rates of 51.1% (95% CI: 50.5-51.7%) and 57.1% (95% CI: 56.5-57.6%) for patients diagnosed in 2005 and 2013 respectively. Three-year survival for patients undergoing major resection also increased from 66.3% (95% CI: 65.6-66.9%) in 2005 to 75.7% (95% CI: 75.1-76.3%) in 2013. High variability was observed across the Trusts. Three-year survival ranged from 46.4% to 70.3% for patients diagnosed between 2011-2013 and 60.0% to 86.6% for those who underwent major resection. There was also variability by cancer site with three-year survival from diagnosis for patients diagnosed with colon cancer between 2011-2013 being 54.9% (95 CI: 54.5-55.3%) and for those diagnosed with rectal cancer 62.3% (95% CI: 61.7-62.8%).
Conclusions- This study identified significant variation in CRC crude survival across the English NHS that need further investigation in order to detect the causes and improve results and practice.
Acknowledgements- This work uses data provided by patients and collected by the NHS. Cancer Research U.K. (CRUK) funded this research and National Cancer Registration and Analysis Service (NCRAS) made the data available for analyses. We would like to thank these organisations, and NHS patients, for making this research possible.
Centralisation of anal cancer surgery in England
Presented at The Association of Coloproctology of Great Britain and Ireland 2019 Annual Meeting.
Abstract:
Background- National guidelines, published in 2004, recommend that anal cancer is managed in specialist centres. Anal cancer multidisciplinary teams (MDTs) should have one or two surgeons performing any salvage surgery (for residual or recurrent disease): this will ensure individual surgeons are performing an adequate number of cases. This study investigates patterns of surgical care for anal cancer in the English NHS before and after publication of this guidance.
Methods- Using the CORECT-R data repository, we identified patients diagnosed with squamous cell anal cancer between 01/01/2000 and 31/12/2013 who subsequently underwent an abdominoperineal excision (APE) within three years of diagnosis. The data were split into 4 time periods according to the date of APE. The number of APEs and number of MDTs performing these operations in each time period were calculated.
Results- There were 664 patients diagnosed with anal cancer between 2000 and 2013 who subsequently had an APE. The median number of days between diagnosis and APE increased over the study period from 165 days to 376 days. The number of APEs increased from 141 in 2000-2003 to 202 in 2012-2015, whilst the number of MDTs performing these operations decreased from 91 to 50. In the most recent period, 6 MDTs performed ≥10 APEs, 10 MDTs performed 5-10 APEs and 34 MDTs performed <5 APEs.
Discussion- These preliminary results suggest that surgery for anal cancer is becoming more centralised over time. Further work will investigate the extent of centralisation within regions and Cancer Alliances, and possible associations with post-surgical outcomes.